Critical Care/Lung Injury
 Critical Care Medicine research at UCSF includes Acute Lung Injury and Sepsis. Both are a major focus for basic and clinical research. The research opportunities include molecular, cell and organ based studies as well as patient based research. In addition, there is an opportunity to participate in phase 2 and 3 clinical trials. UCSF has a long tradition of NIH supported research in sepsis and acute lung injury with a history of being one of the major national and international leaders in both basic and clinical research and pivotal clinical trials.
Critical Care Medicine research at UCSF includes Acute Lung Injury and Sepsis. Both are a major focus for basic and clinical research. The research opportunities include molecular, cell and organ based studies as well as patient based research. In addition, there is an opportunity to participate in phase 2 and 3 clinical trials. UCSF has a long tradition of NIH supported research in sepsis and acute lung injury with a history of being one of the major national and international leaders in both basic and clinical research and pivotal clinical trials.
Several graduates of the UCSF Pulmonary Critical Care training program began their research career as fellows at UCSF and then progressed to receive NHLBI K08 or K23 training awards to launch their successful academic careers at UCSF and other major universities.
Research opportunities in ARDS and Sepsis
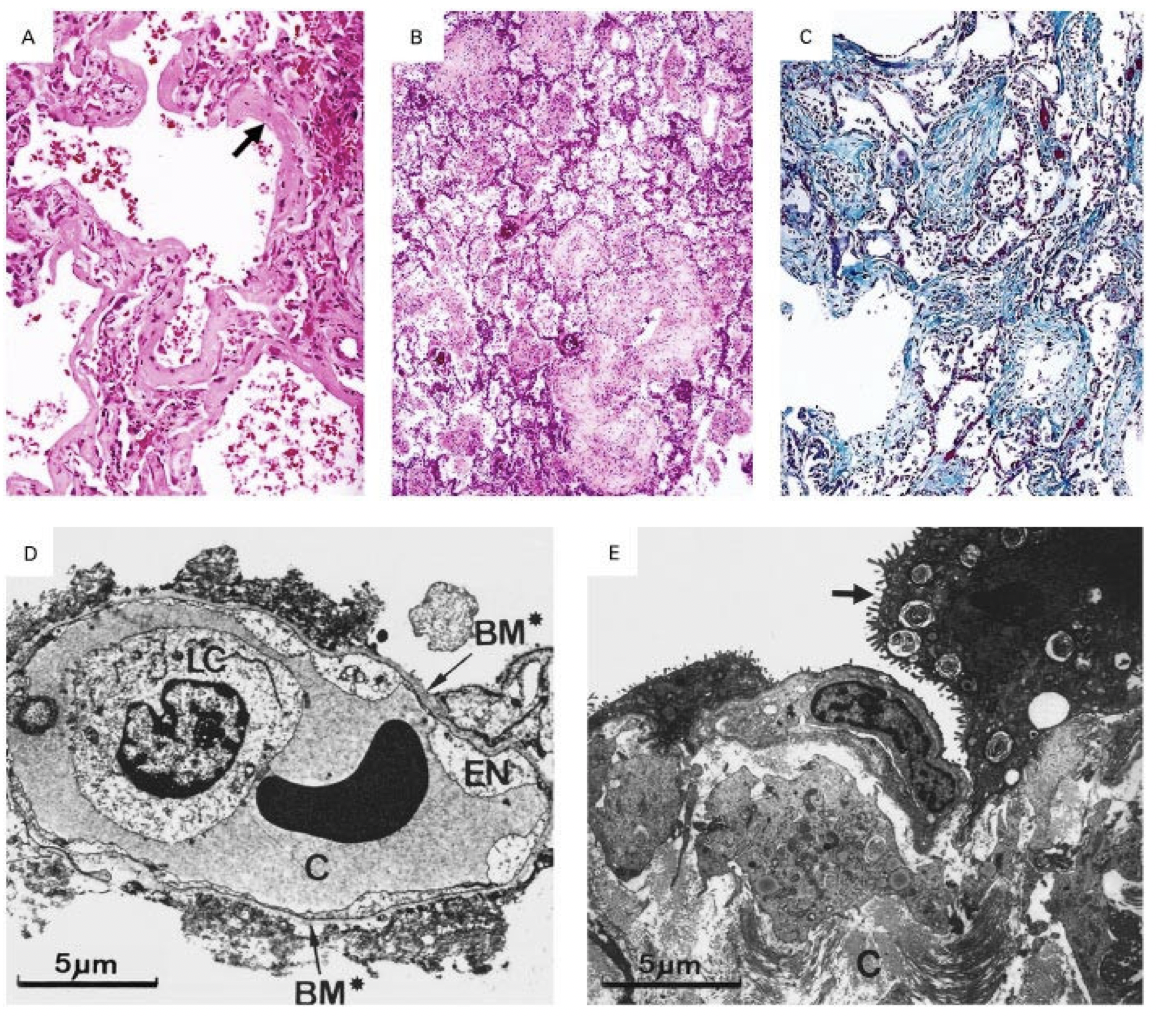
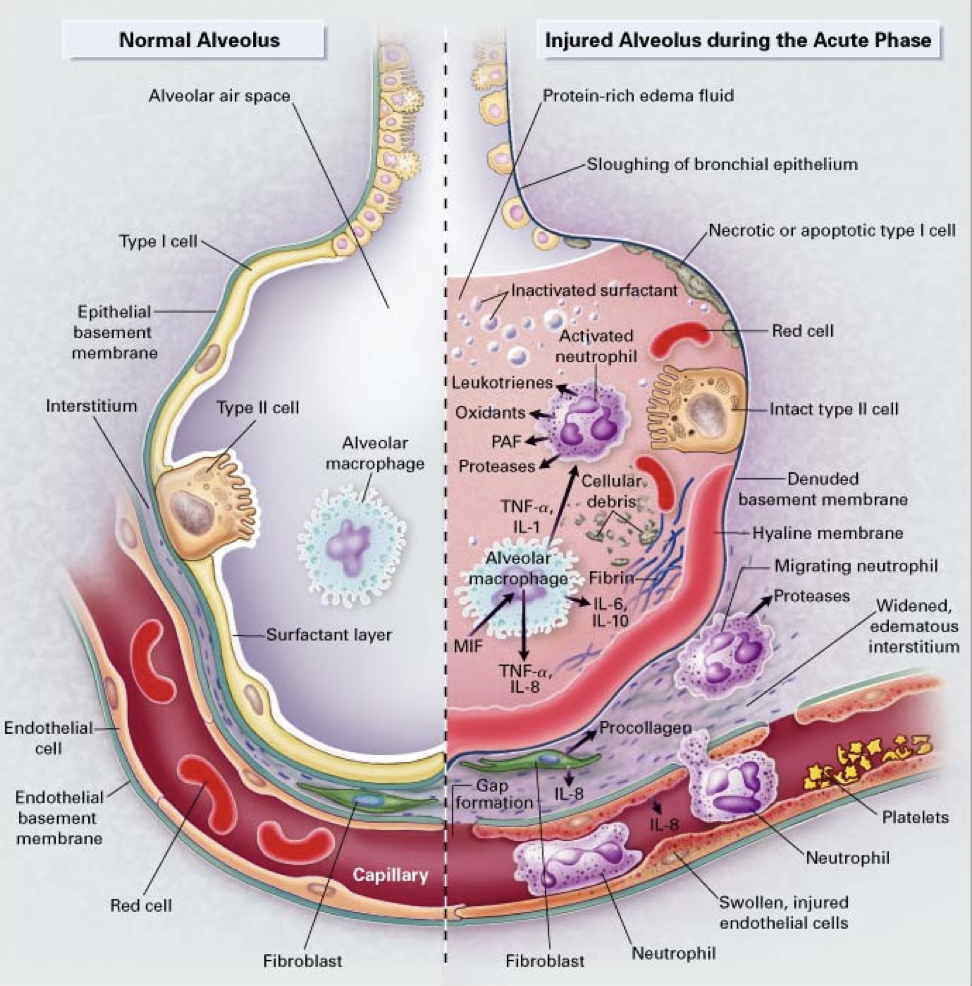 There are exciting research opportunities in laboratory-based studies in Dr. Michael Matthay’s and Dr. Jeff Gotts’ group at Parnassus in the CVRI. The studies include cell-based studies focused on the lung endothelium and the alveolar epithelium, primarily using human cells. In addition, there are clinically relevant mouse models that study the mechanisms of lung injury, including pneumonia and sepsis models. Finally, this laboratory also includes the novel use of the ex vivo perfused human lung preparation to study pathogenesis of lung injury and test new treatments for ARDS (see review in JCI Insight, 2019).
There are exciting research opportunities in laboratory-based studies in Dr. Michael Matthay’s and Dr. Jeff Gotts’ group at Parnassus in the CVRI. The studies include cell-based studies focused on the lung endothelium and the alveolar epithelium, primarily using human cells. In addition, there are clinically relevant mouse models that study the mechanisms of lung injury, including pneumonia and sepsis models. Finally, this laboratory also includes the novel use of the ex vivo perfused human lung preparation to study pathogenesis of lung injury and test new treatments for ARDS (see review in JCI Insight, 2019).
In addition, Mark Looney, MD has an outstanding laboratory and translational based program using clinically relevant mouse models of lung injury with state of the art imaging methods. His animal based studies have also had a strong translational dimension with clinical research studies as well in ARDS.
Dean Sheppard, MD also has an interest in mechanisms of lung injury with mouse based models at his CVRI laboratory.
In addition to the lung injury research, Dr. Gotts directs a laboratory based program to study the effects of cigarette smoke and e-cigarettes in cell culture models as well in vivo studies in mice. This research program is part of a large NHLBI/FDA program project grant.
There is also a strong clinical research group led by Drs. Calfee and Matthay focused on understanding the mechanisms of lung injury and sepsis based on clinical and biologic data, both from secondary analyses of NHLBI clinical trials as well as prospective research in patients at Parnassus and ZSFG hospitals. Dr. Calfee has pioneered a new area of precision medicine in ARDS that is especially relevant for ARDS and for sepsis. She also oversees studies of the role of pathogens in patients with respiratory failure using next generation sequencing in collaboration with Chaz Langelier, MD, as Assistant Professor in Infectious Disease. The clinical research also includes studies of protein biomarkers and transcriptomics of circulating cells in patients with ARDS and sepsis. There are also opportunities to work with Kathleen Liu, MD, PhD who is a nephrologist and critical care attending. Dr. Gotts and Dr. Liu are Co-Directors of the Parnassus Medical ICU.
Approximately 10 years ago, Drs. Calfee and Liu founded a research program titled EARLI (Early Acute Renal and Lung Injury) that identifies patients in the ED who are going to be admitted to the ICU. This EARLI patient cohort has been the basis for several major research studies and extra-mural funding. Dr. Calfee oversees this research program which does recruit patients from Parnassus and ZSFG. Several investigators participate in this program including Antonio Gomez MD, Carolyn Hendrickson, MD, MAS, Kirsten Kangelaris, MD, MAS plus coordinators and fellows.
At ZSFG Dr. Carolyn Hendrickson leads a program focused on studies of ARDS in patients, combining clinical data and biomarkers. She works closely with Drs. Matthay and Clafee. She and Antonio Gomez, MD Co-Direct the MICU at ZSFG.
Clinical Trials
Finally, UCSF has been part of the NHLBI ARDS network clinical trials network since its inception in 1995. The network is now called PETAL (Prevention and Treatment of Acute Lung Injury). The PETAL netwowrk includes identification and recruitment of patients in the ED and the ICU for sepsis and ARDS trials. Dr. Matthay has been the PI from the outset. This network has produced the pivotal trials on low tidal volume (NEJM 2000) and fluid conservative therapy (NEJM, 2006) as well as the recent important trial on neuromuscular blockers for ARDS (NEJM, 2019). Although the California network is based at UCSF, it includes other participating hospitals (Stanford, UCLA, UC Davis and UCSF Fresno). Several co-investigators play a major role in patient recruitment and enrollment, including Carolyn Calfee, MD, MAS, Jeff Gotts, MD, PhD, and Kathleen Liu, MD, PhD. There is also a new phase 2b clinical trial that will begin in 2019 led by Dr. Matthay to test allogeneic bone-marrow derived mesenchymal stromal cells for treatment of ARDS; this trial will be done at both ZSFG and Parnassus. Dr. Hendrickson will be the site investigator at ZSFG for this trial along with faculty in Surgery (Rachael Calcutt, MD, MAS) and Antesthesioogy (Michael Lipnick, MD, MAS).
Mentoring
On balance, there are outstanding research opportunities for fellows interested in research and clinical trials in ARDS and Sepsis. Dr. Matthay has a long history of strong mentoring (UCSF Clinical Research Award, 2006) and Dr. Calfee received the inaugural mentoring award from the Pulmonary-Critical Care Fellows in 2018.
Disease area - ARDS and Sepsis
Basic Research
-
Matthay lab (Parnassus)
-
Gotts Lab (Parnassus)
-
Looney Lab (Parnassus)
-
Sheppard Lab (CVRI)
Clinical Trials
-
Matthay is the PI for NHLBI and DoD trials with major Co-Investigator input from Drs. Calfee, Gotts, Liu and Hendrickson
-
Matthay and Calfee have also led a recent observational study of pulmonary hypertension in ARDS funded by Bayer Pharmaceuticals
Clinical Research
-
Calfee Group (Parnassus and ZSFG)
-
Matthay Group (Parnassus and ZSFG)
-
Hendrickson Group (ZSFG)
Translational research
-
Drs. Calfee, Matthay, Looney, Dr. Hendrickson and Liu
FACULTY
-
Michael A. Matthay, MD (Professor, Medicine and Anesthesia)
-
Carolyn S. Calfee, MD, MAS (Professor, Medicine and Anesthesia)
-
Jeff E. Gotts, MD, PhD (Assistant Professor, Medicine and Anesthesia)
-
Carolyn Hendrickson, MD, MPH (Assistant Professor, Medicine and Anesthesia)
-
Kathleen D. Liu, MD, PhD (Professor, Medicine)
-
Mark Looney, MD (Professor, Medicine and Anesthesia)
-
Dean Sheppard, MD (Professor, Medicine)