Basic Biology
UCSF is one of the leaders in basic lung biology, exploring fundamental principles that govern immunology, stem cell biology, matrix biology, developmental biology, genetics, and cell biology in the lung. Our labs span across multiple campuses, including Parnassus Heights, Mission Bay, ZSFG, and SFVAMC. Below are the labs with their respective research focus.
-
Dean Sheppard Lab
Molecular mechanisms underlying pulmonary fibrosis, roles of TGFbeta activating integrins in suppressing immune responses to tumors and use of synthetic biology to develop cell-based therapies for pulmonary fibrosis. -
Mark Looney Lab
Acute lung inflammation and injury with a focus on the innate immune system including neutrophils, NETs, and platelets. -
Erin Gordon Lab
Understanding the molecular basis for asthma (and allergic disease) genetic risk. -
Mallar Bhattacharya Lab
Understanding how monocytes and macrophages regulate inflammatory responses and provide cues to other cell types in subtissular niches. -
John Fahy Lab
Exploring disease biology in airway diseases such as asthma, CF, and COPD with an emphasis on mechanisms of epithelial cell dysfunction and of mucus gel pathology. -
Paul Wolters Lab
Utilizing novel animal models and translational studies to define cellular and molecular mechanisms that cause lung fibrosis. -
Aparna Sundaram Lab
The role of cellular tethering in smooth muscle force transmission in asthma. -
Kamran Atabai Lab
Understanding the role of cell-mediated collagen degradation in regulating the severity of fibrosis -
Anthony Shum Lab
Basic research using mouse models and human cells to study the pathogenic mechanisms underlying Mendelian autoimmune disorders that affect the lung. -
Ari Molofsky Lab
Defining the cells and signals that control lung type 2 immune responses in health and disease" -
Jeremy Reiter
The Reiter lab investigates the formation and function of cilia in the lung. Motile cilia in the upper airway are critical for protecting the lung from inhaled particles and pathogens. Non-motile primary cilia transduce intercellular signals critical for lung development and homeostasis. This research is helping to uncover the etiology of inherited lung diseases such as Primary Ciliary Dyskinesia (PKD).
-
Pao-Tien Chuang Lab
Molecular mechanisms of lung development, repair and tumorigenesis. -
Hal Chapman Lab
Molecular mechanisms of lung progenitor repair and small-molecule strategies for inhibiting TGF-beta in fibrotic lung disease. -
Maya Kotas Lab
Homeostatic and disease-generating coordination between epithelial and immune cells in the lung and airway. -
Chris Allen Lab
Use of in cutting-edge microscopy to visualize interactions among cells in the lungs and lymphoid organs that ‘prime’ cells for immune responses. -
David Erle Lab
Using regulatory genomics to understand mechanisms of airway epithelial cell reprogramming in asthma. -
Vincent Auyeung Lab
Determining how cellular stress responses in the lung epithelium regulate lung epithelial plasticity and differentiation across lung diseases from asthma to pulmonary fibrosis. -
Feroz Papa Lab
The role of airway epithelial ER Stress/ unfolded protein response in lung diseases. -
Stephen Nishimura Lab
Mechanisms of airway remodeling in COPD. -
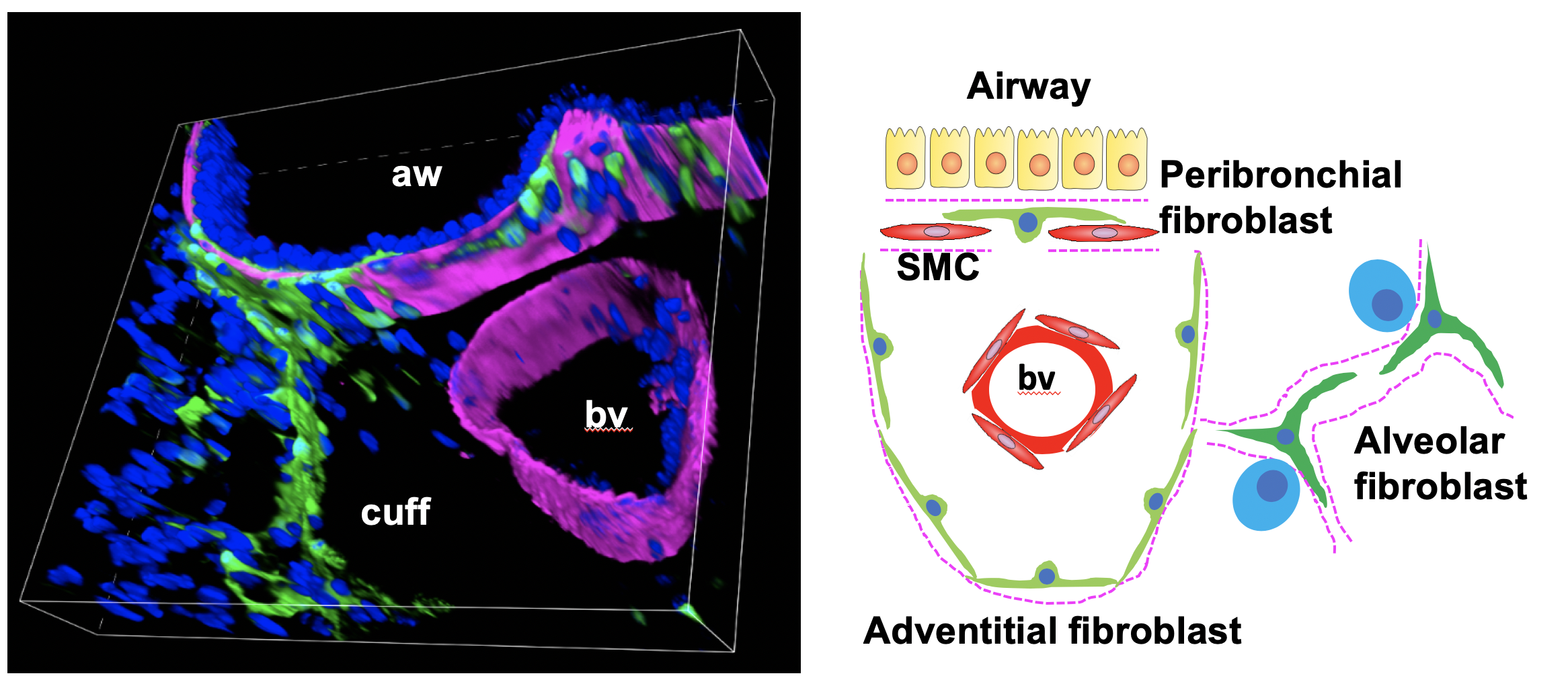
Tien Peng Lab
Mesenchymal-mediated alteration of the stem cell microenvironment and its role in lung diseases. -
Max Krummel Lab
Dynamics of the immune synapse. -
Mark Ansel Lab
The role of MicroRNAs, transcription factors, and epigenetic regulation in control lymphocyte development, differentiation, and function. -
John Greenland Lab
Elucidating mechanisms driving chronic lung allograft dysfunction after lung transplantation, including alloimmune responses and accelerated aging, leveraging multi-omics and transplant models. -
Daniel Calabrese Lab
Understanding the innate immune drivers of ARDS, and acute and chronic lung injury after lung transplantation. Specific foci include NK cells, cytomegalovirus and the role of hypoxia signaling in the airway epithelium. We use multi-omics approaches in human samples and mouse models.