Airway/Allergy/Environmental Disease



 UCSF has a long history of research in allergy and asthma and especially in mechanisms of airway inflammation in asthma. Over the past 50 years, multiple faculty members at UCSF have contributed importantly to current knowledge of the specific cells and mediators that drive allergic inflammation and asthma. Seminal discoveries at UCSF have provided rationale for the treatment of asthma with inhaled anticholinergic drugs and anti-inflammatory drugs such as corticosteroids, leukotriene receptor antagonists, and anti-cytokine therapies (especially anti IL13). UCSF has also been a leader in identifying molecular subtypes of asthma and in developing biomarkers for specific asthma subtypes. Most multicenter asthma research initiatives funded by the NIH include UCSF, which is a participating center for programs such as PRECISE, the Severe Asthma Research Program (SARP), the Asthma and Allergy Research Diseases Cooperative Research Centers (AADCRC), and the Inner City Asthma Consortium. Major asthma cohort studies are also based here, including cohort studies in minority populations that are focused on asthma genetics. Clinical and Translational research in asthma at UCSF occurs on the Parnassus campus (in the UCSF Airway Clinical Research Center (ACRC] and the Sandler Asthma Basic Research [SABRE] program), the Mission Bay campus, at Zuckerberg San Francisco General (ZSFG), and at the San Francisco Veteran Affairs Medical Center (SFVAMC). In addition, UCSF has significant basic research into the pathogenesis of allergic inflammation more generally. This basic research is carried out within the Division of Pulmonary, Critical Care, Allergy and Sleep Medicine and is also undertaken in collaborating laboratories in other Divisions and Schools at UCSF. Some of these collaborators are organized under the umbrella of SABRE. Below are examples of projects related to ongoing basic research on Allergy at UCSF.
UCSF has a long history of research in allergy and asthma and especially in mechanisms of airway inflammation in asthma. Over the past 50 years, multiple faculty members at UCSF have contributed importantly to current knowledge of the specific cells and mediators that drive allergic inflammation and asthma. Seminal discoveries at UCSF have provided rationale for the treatment of asthma with inhaled anticholinergic drugs and anti-inflammatory drugs such as corticosteroids, leukotriene receptor antagonists, and anti-cytokine therapies (especially anti IL13). UCSF has also been a leader in identifying molecular subtypes of asthma and in developing biomarkers for specific asthma subtypes. Most multicenter asthma research initiatives funded by the NIH include UCSF, which is a participating center for programs such as PRECISE, the Severe Asthma Research Program (SARP), the Asthma and Allergy Research Diseases Cooperative Research Centers (AADCRC), and the Inner City Asthma Consortium. Major asthma cohort studies are also based here, including cohort studies in minority populations that are focused on asthma genetics. Clinical and Translational research in asthma at UCSF occurs on the Parnassus campus (in the UCSF Airway Clinical Research Center (ACRC] and the Sandler Asthma Basic Research [SABRE] program), the Mission Bay campus, at Zuckerberg San Francisco General (ZSFG), and at the San Francisco Veteran Affairs Medical Center (SFVAMC). In addition, UCSF has significant basic research into the pathogenesis of allergic inflammation more generally. This basic research is carried out within the Division of Pulmonary, Critical Care, Allergy and Sleep Medicine and is also undertaken in collaborating laboratories in other Divisions and Schools at UCSF. Some of these collaborators are organized under the umbrella of SABRE. Below are examples of projects related to ongoing basic research on Allergy at UCSF.
ACRC: Airway Clinical Research Center
The Airway Clinical Research Center (ACRC) investigates and validates new and existing therapies for airway conditions. Examples of airway conditions include asthma, Chronic Obstructive Pulmonary Disease (COPD), and Cystic Fibrosis.
Learn more about ACRC's studies and sign up for clinical trials on the ACRC website.
Contact Us
505 Parnassus Avenue, M1329
San Francisco, CA 94143-0130
(T): 415-502-4849
(F): 415-502-7814
(E): [email protected]
Allergy and Asthma
 UCSF has a long history of research in allergy and asthma and especially in mechanisms of airway inflammation in asthma. Over the past 50 years, multiple faculty members at UCSF have contributed importantly to current knowledge of the specific cells and mediators that drive allergic inflammation and asthma. Seminal discoveries at UCSF have provided rationale for the treatment of asthma with inhaled anticholinergic drugs and anti-inflammatory drugs such as corticosteroids, leukotriene receptor antagonists, and anti-cytokine therapies (especially anti IL13). UCSF has also been a leader in identifying molecular subtypes of asthma and in developing biomarkers for specific asthma subtypes. Most multicenter asthma research initiatives funded by the NIH include UCSF, which is a participating center for programs such as PRECISE, the Severe Asthma Research Program (SARP), the Asthma and Allergy Research Diseases Cooperative Research Centers (AADCRC), and the Inner City Asthma Consortium. Major asthma cohort studies are also based here, including cohort studies in minority populations that are focused on asthma genetics. Clinical and Translational research in asthma at UCSF occurs on the Parnassus campus (in the UCSF Airway Clinical Research Center (ACRC] and the Sandler Asthma Basic Research [SABRE] program), the Mission Bay campus, at Zuckerberg San Francisco General (ZSFG), and at the San Francisco Veteran Affairs Medical Center (SFVAMC). In addition, UCSF has significant basic research into the pathogenesis of allergic inflammation more generally. This basic research is carried out within the Division of Pulmonary, Critical Care, Allergy and Sleep Medicine and is also undertaken in collaborating laboratories in other Divisions and Schools at UCSF. Some of these collaborators are organized under the umbrella of SABRE. Below are examples of projects related to ongoing basic research on Allergy at UCSF.
UCSF has a long history of research in allergy and asthma and especially in mechanisms of airway inflammation in asthma. Over the past 50 years, multiple faculty members at UCSF have contributed importantly to current knowledge of the specific cells and mediators that drive allergic inflammation and asthma. Seminal discoveries at UCSF have provided rationale for the treatment of asthma with inhaled anticholinergic drugs and anti-inflammatory drugs such as corticosteroids, leukotriene receptor antagonists, and anti-cytokine therapies (especially anti IL13). UCSF has also been a leader in identifying molecular subtypes of asthma and in developing biomarkers for specific asthma subtypes. Most multicenter asthma research initiatives funded by the NIH include UCSF, which is a participating center for programs such as PRECISE, the Severe Asthma Research Program (SARP), the Asthma and Allergy Research Diseases Cooperative Research Centers (AADCRC), and the Inner City Asthma Consortium. Major asthma cohort studies are also based here, including cohort studies in minority populations that are focused on asthma genetics. Clinical and Translational research in asthma at UCSF occurs on the Parnassus campus (in the UCSF Airway Clinical Research Center (ACRC] and the Sandler Asthma Basic Research [SABRE] program), the Mission Bay campus, at Zuckerberg San Francisco General (ZSFG), and at the San Francisco Veteran Affairs Medical Center (SFVAMC). In addition, UCSF has significant basic research into the pathogenesis of allergic inflammation more generally. This basic research is carried out within the Division of Pulmonary, Critical Care, Allergy and Sleep Medicine and is also undertaken in collaborating laboratories in other Divisions and Schools at UCSF. Some of these collaborators are organized under the umbrella of SABRE. Below are examples of projects related to ongoing basic research on Allergy at UCSF.
Basic Research
-
Using regulatory genomics to understand mechanisms of airway epithelial cell reprogramming in asthma. Erle Lab
-
Understanding the molecular basis for asthma (and other allergic disease) genetic risk. Gordon Lab
-
The role of cellular tethering in smooth muscle force transmission in asthma. Sundaram Lab
-
Macrophage activation in mouse models of airway hyper-responsiveness. Bhattacharya Lab
-
Cellular targets of the unfolded protein response that contribute to airway hyper-responsiveness in models of allergic asthma Sheppard and Papa Labs
-
The role of MicroRNAs in airway epithelial mucin production. Woodruff Lab
-
The role of Mfge8 in regulating smooth muscle function and the inflammatory response in allergic airway disease. Atabai Lab
-
The role of group 2 innate lymphoid cells in tissue maintenance and pathology. Locksley Lab
-
Molecular mechanism and functional studies of dendritic cells in asthma. Shin Lab
-
The role of MicroRNAs, transcription factors, and epigenetic regulation in control lymphocyte development, differentiation, and function. Ansel Lab
-
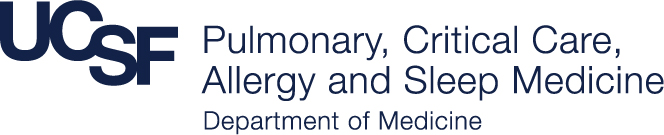
The use of in cutting-edge microscopy to visualize interactions among cells in the lungs and lymphoid organs that ‘prime’ cells for immune responses. Allen Lab
Clinical Trials and Clinical/Translational Research
-
Precision Interventions for Severe and/or Exacerbation Prone Asthma (PrecISE) Network: this 10-center adaptive clinical trial aims to develop biomarker-informed treatment for severe forms of asthma. Fahy Lab or ACRC
-
Severe Asthma Research Program (SARP) - A longitudinal cohort study of Severe Asthma: this seven-center cohort study aims to improve the understanding of severe asthma in order to develop better treatments. Fahy Lab or ACRC
-
CF And Effects of Drugs Mixed Ex Vivo With Sputum for Mucolytic Treatment (CADET); This is a drug development program that aims to bring a novel mucolytic drug to the clinic for treatment of mucus-associated lung disease. Fahy Lab or ACRC
-
The UCSF Asthma Collaboratory has created the largest gene-environment study of asthma in minority children in the U.S. We were recently funded by the NIH to create PRIMERO (Puerto Rican Infant Metagenomic and Epidemiologic study of Respiratory Outcomes), a birth cohort to study the early life origins of severe respiratory disease and asthma in 3,000 Puerto Rican mothers and their newborns. UCSF Asthma Collaboratory
-
Focal type 2 niches in the asthma airway. This is a mechanism-oriented clinical study designed to discover mechanisms of focal type 2 inflammation and mucus pathology in severe forms of asthma. Fahy Lab or ACRC
-
ACE: Allergen Challenge for Evoked Phenotypes in Asthma. A mechanism-oriented human segmental lung allergen challenge study designed to identify epithelial and immune responses to allergen in the airway in asthma using genomics and single cell methods. Woodruff Lab
-
SEARCH/PISA: Single-site, longitudinal, mechanistic, induced sputum and bronchoscopy study of asthmatic and healthy human participants to identify differences in airway epithelial epigenetic enhancer signatures in asthma, and temporal stability of sputum and airway epithelial gene expression measures of inflammation. Bhakta Lab
-
Applied statistical genetics/studies of genetic and environmental risk factors for asthma in minority children. White Lab
-
VA Airborne Hazards Collaborative Network is a congressionally mandated multicenter project to study post-deployment respiratory health effects of exposure to combat-related air pollutants including irritant-induced asthma and reactive airway disease syndrome. Arjomandi Lab
-
Collaborative microbiome studies (with Susan Lynch, PhD, G-I Division) of the role of the gut and airway microbiome, metagenome, and metabolome in the development, phenotype, and responsiveness to therapy of asthma. Homer Boushey
-
Impact of early-life adversity, socioeconomic and structural determinants of health on asthma and asthma-related health outcomes. Thakur Group
COPD/Emphysema
UCSF has been a prominent site for research on Chronic Obstructive Pulmonary Diseases (COPD), including Chronic Bronchitis and Emphysema, for more than 40 years. Our faculty are involved in studies of the basic pathogenic mechanisms of COPD, genetics, epidemiology, early diagnosis, and treatment, as well as studies on the role of smoking, air pollution, and exposure to fumes from biomass fuels. The multicenter COPD research initiatives funded by the NIH at UCSF include SPIROMICS II (a multicenter study directed by UCSF) and the COPD clinical trials organized by the Pulmonary Trials Consortium of the NIH and the American Lung Association.
Basic Research
-
Mechanisms of airway remodeling in COPD. Nishimura Lab
-
Studying the role of the stem cell niche in emphysema pathogenesis. Peng Lab
Clinical Trials and Clinical/Translational Research
-
Flight Attendants Health Study is a single-center study of the physiologic, radiographic, and inflammatory sequelae of prolonged and heavy exposure to secondhand tobacco smoke in nonsmokers. Arjomandi Lab
-
Secondhand Smoke Respiratory Health Study is a single-center placebo-controlled crossover randomized controlled trial of bronchodilators in nonsmokers at risk for COPD due to prolonged exposure to secondhand tobacco smoke who have air trapping and dynamic hyperinflation yet preserved spirometry. Arjomandi Lab
-
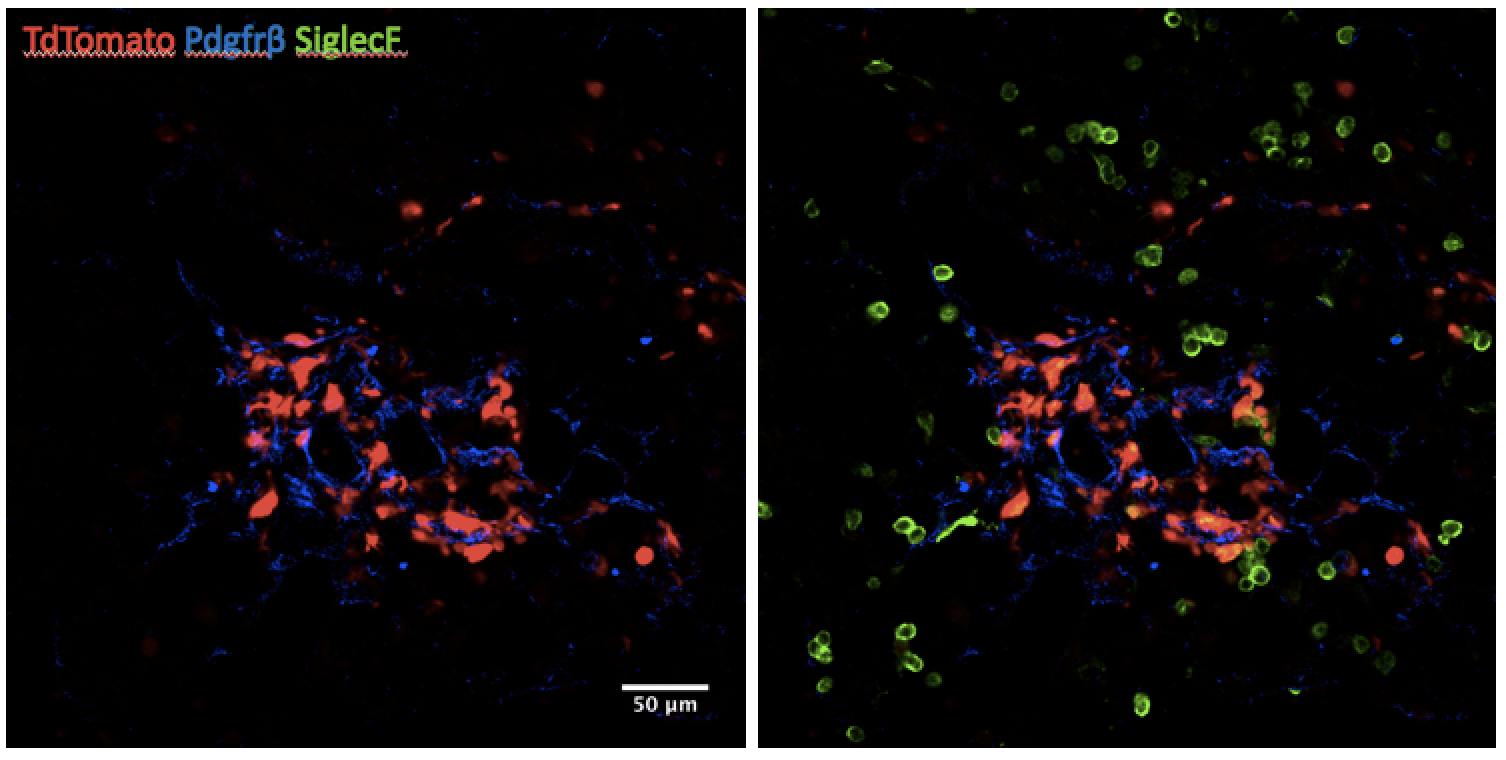
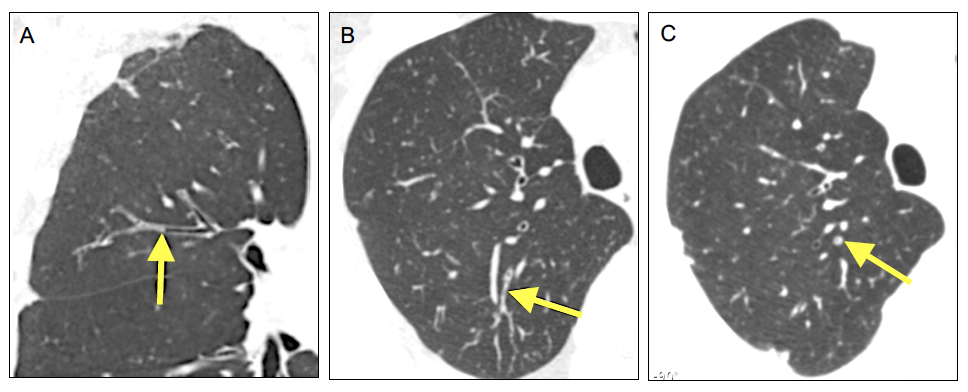
Identification of molecular phenotypes of COPD. Woodruff Lab and Christenson Lab
-
Studies of host/pathogen interactions in COPD exacerbations. Christenson Lab
-
SPIROMICS I and II: The Subpopulations and Intermediate Outcome Measures in COPD Study. A multi-center longitudinal cohort study designed to identify subpopulations of COPD and investigate the biological underpinnings of COPD progression and exacerbation. Woodruff Lab or ACRC
-
RETHINC Study: Redefining Therapy in Early COPD. A multi-center randomized controlled clinical trial of bronchodilators in current and former smokers who have symptoms of COPD despite preserved spirometry Woodruff Lab or ACRC
-
LEEP Study: A multi-center randomized controlled trial of Losartan to slow the progression of emphysema. Lazarus group or ACRC
-
INSIGHT COPD Study: A multi-center randomized controlled trial of a weight loss program in overweight patients with COPD. Lazarus group or ACRC
-
Delivery of evidence-based interventions within safety-net settings to address asthma and COPD disparities. Thakur Group
-
VA Airborne Hazards Collaborative Network is a congressionally mandated multicenter project to study post-deployment respiratory health effects of exposure to combat-related air pollutants including early and mild COPD. Arjomandi Lab
-
Da VINCI project is an epidemiological study of VA nationwide electronic health records that uses supervised and unsupervised (machine learning) approaches to discover the clinical phenotypes of complex respiratory diseases such as COPD and to generate mechanism-oriented hypotheses. Arjomandi Lab
-
Understanding the endotype of the “susceptible smoker” in pre-COPD. This is currently a single-center pilot study (approved to become a multicenter ancillary study associated with SPIROMICS II) to explore the role of lung innate immunity in pre-COPD by molecular phenotyping of lung macrophages using single-cell proteomics (mass cytometry) and genomics. Arjomandi Lab
-
CO3PD Study: modeling exacerbation using ozone exposure in patients with COPD. This is a controlled human exposure study to model pollutant-induced exacerbation in patients with moderate to severe COPD to investigate the role of resident versus incoming lung macrophages in susceptibility to develop COPD exacerbation. Arjomandi Lab or Human Exposure Lab
Cystic Fibrosis
UCSF has been a major center for cystic fibrosis research for more than 25 years, receiving funding from the Cystic Fibrosis Foundation, National Institutes of Health, and other agencies. For example, the Cystic Fibrosis Research and Development program at UCSF, one of the few basic research centers sponsored by the Cystic Fibrosis Foundation, has long focused on understanding the biology of alterations in the cystic fibrosis transmembrane conductance regulator (CFTR) protein and identifying molecular approaches to correct fundamental defects in CFTR that lead to disease. In addition, UCSF physicians and researchers are engaged in many other areas of cystic fibrosis research. For adults with CF cared for at our Center, clinical research studies led by UCSF investigators provide opportunities for patients to participate as research study volunteers. Some areas of recent and ongoing research investigation are highlighted below.
-
Clinical trials of new therapies for CF: Mary Ellen Kleinhenz
-
Understanding the basis of abnormal mucus properties and hypersecretion in CF: Fahy Lab
-
Developing new therapies and studying lung pathogenesis mechanisms in cystic fibrosis. Verkman Lab
Clinical Trials and Clinical/Translational Research
-
Understanding how abnormal mucus forms in diseases of the airways such as asthma and cystic fibrosis “the MUCGAL Study”: Fahy Lab
-
Cystic Fibrosis Foundation Therapeutics Development Network: UCSF has been selected to participate in the phase 2 clinical trial, VX 18-NGC-104 to evaluate safety and effective of triple combination CFTR modulators in patients with gating and residual function mutations. Jon Singer, Ngoc Ly
The Human Exposure Laboratory (HEL)
The UCSF Human Exposure Laboratory (HEL) conducts research to better understand how air pollutants affect human health. Historically, HEL conducted controlled human exposure studies using an environmental chamber to investigate the effects of pollutants such as ozone, particulate matter, smoke, and secondhand tobacco smoke. Currently, HEL focuses on comprehensive exposure assessment, epidemiological research, advanced cardiopulmonary physiologic experimentation, and translational research using human biological samples.
Learn more about HEL’s studies and participate in clinical research studies on the HEL website.
FACULTY